"Nothing About Us Without Us"
1 de Outubro de 2022, 15:00 - sem comentários ainda
Before we redesigned our website a couple of years ago, we took pains to have some users show us how they navigate our content or complete specific tasks like leaving a comment or listening to a podcast. We queried them about what they liked or didn’t like about how our content is presented. And we took onboard their experiences and designed a site and a magazine based on that feedback.
So when I read this month’s cover story by Britt Young about using a variety of high- and low-tech prosthetic hands, I was surprised to learn that much bionic-hand development is conducted without taking the lived experience of people who use artificial hands into account.
I shouldn’t have been. While user-centered design is a long-standing practice in Web development, it doesn’t seem to have expanded deep into other product-development practices. A quick search on the IEEE Xplore Digital Library tallied less than 2,000 papers (out of 5.7 million) on “user-centered design.” Five papers bubbled up when searching “user-centered design” and “prosthesis.”
Young, who is working on a book about the prosthetics industry, was in the first cohort of toddlers fitted with a myoelectric prosthetic hand, which users control by tensing and relaxing their muscles against sensors inside the device’s socket. Designed by people Young characterizes as “well-intentioned engineers,” these technologically dazzling hands try to recreate in all its complex glory what Aristotle called “the instrument of instruments.”
“It’s more important that we get to live the lives we want, with access to the tools we need, than it is to make us look like everyone else.”
While high-tech solutions appeal to engineers, Young makes the case that low-tech solutions like the split hook are often more effective for users. “Bionic hands seek to make disabled people ‘whole,’ to have us participate in a world that is culturally two-handed. But it’s more important that we get to live the lives we want, with access to the tools we need, than it is to make us look like everyone else.”
As Senior Editor Stephen Cass pointed out to me, one of the rallying cries of the disabled community is “nothing about us, without us.” It is a response to a long and often cruel history of able-bodied people making decisions for people with disabilities. Even the best intentions don’t make up for doing things for disabled people instead of with them, as we see in Young’s article.
Assistive and other technologies can indeed have huge positive impacts on the lives of people with disabilities. IEEE Spectrum has covered many of these developments over the decades, but generally speaking it has involved able-bodied journalists writing about assistive technology, often with the perspective of disabled people relegated to a quote or two, if it was included at all.
We are fortunate now to have the chance to break that pattern, thanks to a grant from the IEEE Foundation and the Jon C. Taenzer Memorial Fund. With the grant, Spectrum is launching a multiyear fellowship program for disabled writers. The goal is to develop writers with disabilities as technology journalists and provide practical support for their reporting. These writers will investigate not just assistive technologies, but also look at other technologies with ambitions for mass adoption through a disability lens. Will these technologies be built with inclusion in mind, or will disabled people be a literal afterthought? Our first step will be to involve people with disabilities in the design of the program, and we hope to begin publishing articles by fellows early next year.
This article appears in the October 2022 print issue.
The Electric Purple Snake-Oil Machine
30 de Setembro de 2022, 15:00 - sem comentários ainda
The violet ray machine has an awesome name that conjures up images of cartoon supervillains taking out Gotham, but its actual history is even odder—and it includes a superhero, not a villain.
The technology underpinning the machine begins with none other than Nikola Tesla and his eponymous coil. After Tesla and others made some refinements to the device, an influential clairvoyant named Edgar Cayce popularized violet ray machines for treating just about every kind of ailment—rheumatism and nervous conditions, acne and baldness, gonorrhea and prostate troubles, brain fog and writer’s cramp. Even Wonder Woman had her own health-restoring Purple Ray device. During the first half of the 20th century, a number of companies manufactured and sold the machines, which became ubiquitous for a time. And yet the scientific basis for the healing effects of violet rays was scant. So what accounted for their popularity?
The cutting-edge tech of the violet ray machine
Violet ray machines employ a Tesla coil, also known as a resonance transformer, to produce a high-frequency, low-current beam, which is then applied to the skin. Nikola Tesla kicked off this line of invention after traveling to Paris during the summer of 1889 to attend the Exposition Universelle. There he learned of Heinrich Hertz’s electromagnetic discoveries. Intrigued, Tesla returned to New York City to run some experiments of his own. The result was the Tesla coil, which he envisioned being used for wireless lighting and power. In April 1891, he applied for a U.S. patent for a “System of Electric Lighting,” which he received two months later. It would be the first in a series of related patents that spanned more than a decade.
In May of that year, Tesla unveiled his wondrous invention to members of the American Institute of Electrical Engineers, during a lecture on his “Experiments with Alternate Currents of Very High Frequency and Their Application to Methods of Artificial Illumination.” He continued to test different circuit configurations and patented some (but not all) of his improvements, such as a “Means for Generating Electric Currents,” U.S. Patent No. 514,168. After more years of tinkering, Tesla perfected his resonance transformer and was granted U.S. Patent No. 1,119,732 for an “Apparatus for Transmitting Electrical Energy” on 1 December 1914.
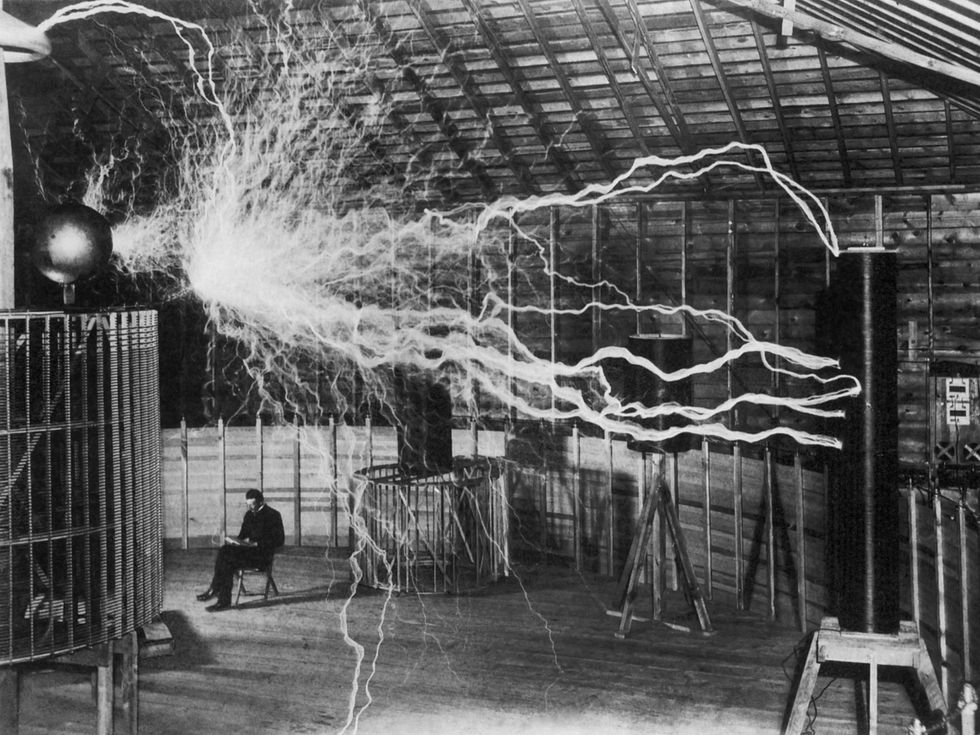 Nikola Tesla envisioned his eponymous coil being used for wireless lighting and power. It was also at the heart of the violet ray machine. Stocktrek Images/Getty Images
Nikola Tesla envisioned his eponymous coil being used for wireless lighting and power. It was also at the heart of the violet ray machine. Stocktrek Images/Getty Images
Tesla promoted the
medical use of the electromagnetic spectrum, suggesting to physicians that different voltages and currents could be used to treat a variety of conditions. His endorsement came at a time when trained doctors as well as shrewd hucksters were already experimenting with electrotherapy and ultraviolet light to help patients or to make a buck, depending on your perspective.
The market was perfectly primed for the violet ray machine, in other words. Tesla himself never commercialized a medical device based around his coil, but others did. The French physician and electrophysiologist Jacques-Arsène d’Arsonval modified Tesla’s design to make the device safer for human use. It was further improved by another French doctor and electrotherapy researcher, Paul Marie Oudin. In 1893, Oudin crafted the first working prototype of what eventually became the violet ray machine. Four years later, Frederick Strong developed an American version.
An influential clairvoyant named Edgar Cayce popularized violet ray machines for treating just about every kind of ailment—rheumatism and nervous conditions, acne and baldness, gonorrhea and prostate troubles, brain fog and writer’s cramp.
Another charismatic individual gets credit for popularizing the device: the psychic
Edgar Cayce. As a young adult, Cayce reportedly lost his voice for over a year. No doctor could cure him, and in desperation he underwent hypnosis. He not only regained the ability to speak, he also began suggesting medical advice and homeopathic remedies. Cayce, who claimed to have had visions from childhood, became a professional clairvoyant, and for the next 40 years he dispensed his wisdom through psychic readings. Out of more than 14,000 recorded readings, Cayce mentioned the violet ray machine almost 900 times. In case you doubt his status as an influencer, Cayce counted Thomas Edison, composer George Gershwin, and U.S. president Woodrow Wilson among his clients.
Was there nothing the violet ray machine couldn’t cure?
The popularity of violet ray machines exploded after 1915, once all of the components for a portable device could be easily manufactured. They could be plugged into a lamp or wall socket or wired to a battery—remember that most homes and businesses in the early 20th century were not yet electrified, and so most manufacturers offered both alternating and direct current options. The machine’s handheld wand consisted of a Tesla coil wrapped in an insulating material, such as Bakelite. The coil produced 1 to 2 kilovolts, which charged a condenser, and then discharged at a rate between 4 to 10 kilohertz when passed over the skin. A voltage selector controlled the intensity of the spark, creating anything from a mild sensation to something quite intense. This video shows the sparks coming from an antique machine:
Glass electrodes—partially evacuated glass tubes known as Geissler tubes—could be inserted into the wand. These came in different shapes depending on their intended use. For example, a rake-shaped attachment worked to massage the scalp, while a narrow tube could be inserted into the mouth, nose, or another orifice. The high voltage ionized the gas within the glass tube, creating the purple glow that gave the device its name.
Numerous manufacturers sprang up to produce the portable machines, including Detroit’s Renulife Electric Co. Founded by inventor James Henry Eastman in 1917, Renulife sold different models for different uses. According to company literature, Model M was its most popular general-purpose product, while Model D was for dentistry, and the tricked-out Model R [pictured at top] had finer regulation of current and a built-in ozone generator to help with head and lung congestion.
In 1917, editors at the Journal of the American Medical Association reported that a violet ray generator certainly couldn’t treat “practically every ailment known to mankind,” as one manufacturer had claimed.
Instructions for the violet ray machines manufactured by Charles A. Branston Ltd. contain an alphabetical list of disorders that could be treated, from abscess to writer’s cramp, with dozens of other ailments in between. Like the Renulife products, the Branston machines also came in different flavors. The Branston machine’s high-frequency mode had germicidal effects and purportedly could be used to cure infections as well as relieve pain. Sinusoidal mode was used to gently massage away nervousness and paralysis. Ozone mode was for inhaling, to treat lung disorders. The Branston devices ranged in price from US $30 for the Model 5B (high-frequency mode only) to $100 for the Model 29 (which had all three modes).
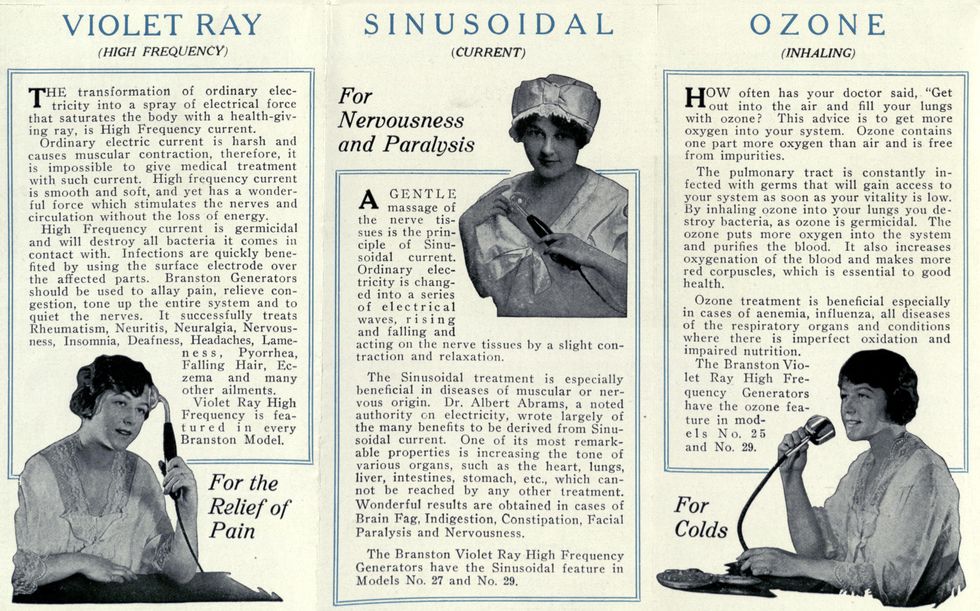 The violet ray machines made by Charles A. Branston Ltd. had different modes for treating a wide variety of ailments.Historical Medical Library/College of Physicians of Philadelphia
The violet ray machines made by Charles A. Branston Ltd. had different modes for treating a wide variety of ailments.Historical Medical Library/College of Physicians of Philadelphia
During the first half of the 20th century, manufacturers marketed the machines to doctors and consumers alike. By the time Wonder Woman debuted in her own comic book in June 1942, the violet ray machine was a well-known household technology. So it wasn’t too surprising that the superhero had a machine of her own.
In the very first issue, Wonder Woman’s future love interest, Steve Trevor, is grievously injured in a plane crash. Seeking to cure his wounds, Diana works tirelessly for five days to complete her Purple Ray machine—but she’s too late. Trevor has died. Undeterred, Diana bathes her patient in the glowing light of the machine. The result might have embarrassed even the admen who wrote the promotional copy for Branston’s products: Wonder Woman’s Purple Ray brings Trevor back to life.
Science frowns on the violet ray machine
Despite their popularity, the machines didn’t fare quite as well within the medical establishment. In 1917, editors at the Journal of the American Medical Association reported that a violet ray generator certainly couldn’t treat “practically every ailment known to mankind,” as one manufacturer had claimed. Although the devices emitted a violet color, they were not in fact emitting ultraviolet light, or at least not in amounts that would be beneficial. In 1951, a Maryland district court ruled against a company named Master Appliances in a libel suit. The charge was misbranding, and the court found that the device was not an effective treatment nor capable of producing the claimed results. At the time, Master Appliances was one of the last manufacturers of violet ray machines in the United States, and the ruling effectively ended production in this country.
And yet you can still buy violet ray machines today—both the antique variety and its modern equivalent. Today’s units are mainly marketed to aestheticians or sold for home use, and some dermatologists are not ready to categorically dismiss their benefits. Although they probably won’t cure indigestion or gray hair, the high frequency can dry out the skin and ozone does kill bacteria, so the machines may help treat acne and other skin conditions. Plus, there’s the placebo effect. As with all consumer electronics for which outrageous claims are made, let the buyer beware.
Part of a continuing series looking at photographs of historical artifacts that embrace the boundless potential of technology.
An abridged version of this article appears in the October 2022 print issue.
Monitoring Parkinson’s Patients at Home Could Improve Disease Management
29 de Setembro de 2022, 17:43 - sem comentários ainda
A radar device the size of a Wi-Fi router could help continuously monitor Parkinson’s disease in patients from afar as they go about their lives at home. By using radio waves to track the gait of Parkinson’s patients, the device should help doctors assess the effectiveness of medications, see how the disease is progressing, and create better treatment plans.
Parkinson’s disease is a chronic, progressive brain disorder that affects motor function, causing tremors, impaired balance, and the risk of falls and injuries. There is no cure for it and patients rely on medications to control symptoms.
Patients then have to visit clinics regularly so specialists can assess their motor and nonmotor symptoms to determine how they are responding to the drugs. The gold-standard test used to assess Parkinson’s disease is the Unified Parkinson’s Disease Rating Scale (UPDRS) in which a patient’s motor skills are evaluated and scored based on a number of physical exercises. But this type of assessment isn’t ideal and can be affected by things like the patient being tired or the subjectivity of the evaluator.
That’s if patients even make it to the clinics in the first place. About 40 percent of patients with Parkinson’s are not seen by neurologists or Parkinson’s specialists, because these care providers are concentrated in medical centers in urban areas. Those suffering from advanced Parkinson’s often have problems traveling to these medical centers due to old age, limited mobility, impaired cognition, and decreased driving ability.
An objective and accurate way to continuously assess Parkinson’s at home could lead to better medical care and also help researchers develop new drugs to control the disorder, says Yingcheng Liu, a Ph.D. candidate in the electrical engineering and computer science department at MIT. One way to do that is to ask patients to wear sensors or measure themselves. But Liu and Guo Zhang of MIT, along with neurologists at the University of Rochester Medical Center wanted to develop a touchless, passive system. So they decided to use radio waves.
Their device, reported in the journal Science Translational Medicine, is the size of a Wi-Fi router, but it transmits radio signals at a thousandth of the power. “Our device works like a low-power home human radar,” Liu says.
An objective and accurate way to continuously assess Parkinson’s at home could lead to better medical care and also help researchers develop new drugs to control the disorder.
The low-power signals can travel through walls and objects, but they reflect off the human body because of its water content. The device collects the signals and sends them to Amazon Cloud where they are analyzed by the advanced signal-processing and machine-learning algorithms that the researchers developed.
Based on the signals, the algorithms extract a patient’s walking movements and trajectories through the home. From these trajectories, Liu says the researchers can calculate the person’s walking speed and evaluate its correlation with Parkinson’s severity, disease progression, and medication response.
The team tested the device by using it to monitor 34 participants with Parkinson’s disease and 16 healthy control subjects continuously in their homes for months. They found that the calculated walking speed correlated with scores on the standard test used today to measure disease severity.
But the at-home gait speed was more sensitive at tracking disease progression over time. “We found that those with Parkinson’s disease had a faster rate of decline in gait speed over time than those without,” Liu says.
What’s more, the device was able to detect the fluctuations in patients’ walking speed in response to medication over the course of the day. Typically, patients have to record these fluctuations in diaries so that doctors can adjust their treatment plans. Being able to detect them remotely using the radar device takes the burden off the patients, the researchers say.
They now need to make the algorithms more robust and efficient, and they plan to test the device and methods on a larger population. Liu says he also wants to analyze more gait parameters such as stride length and swing length. “I will try to combine both gait and sleep to study Parkinson’s in a more holistic aspect,” he says. “Also, there are many other diseases that result in gait dysfunction, such as cancer. I will also study these diseases.”
AI Matches Doctors in Screening for Tuberculosis
24 de Setembro de 2022, 14:00 - sem comentários ainda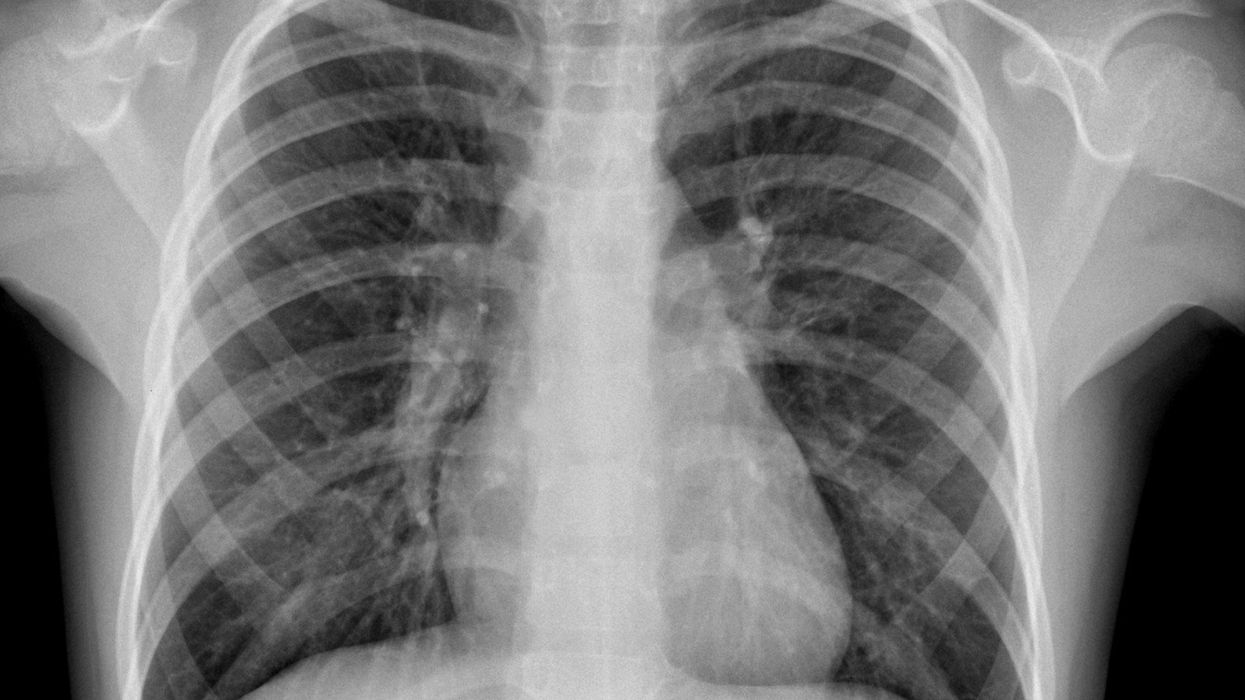
A killer could be stopped cold—or at least be limited in its deadly toll—thanks to AI.
Apart from COVID-19, tuberculosis (TB) is the leading cause of death by an infectious disease worldwide, despite being largely preventable and treatable. While the World Health Organization (WHO) recommends using chest X-rays to help identify likely cases of TB, many health-care centers lack adequate radiologists to interpret these X-rays. In a study published on 6 September in the journal Radiology, researchers at Google along with colleagues from India, South Africa, and Zambia showed that their deep-learning algorithm could identify cases of TB from chest X-rays as well as radiologists could.
“From a global health standpoint, understanding how to efficiently and effectively identify people living with TB” is extremely valuable, said Dr. Christopher Hoffmann—an associate professor of medicine in the division of infectious disease at the Johns Hopkins University School of Medicine—who was not involved in the study.
To train their algorithm, the researchers used more than 165,000 chest X-ray images from 22,000 patients in several European countries, China, India, South Africa, and Zambia. The AI itself had three components—a cropping system, which helped the algorithm analyze the correct part of the image, a smart image-analysis routine, and a final part that combined the two to make the final decision. The algorithm sorts the images into three categories: normal, TB, or abnormal but not TB. As a result it could potentially help even patients who might not have TB but still require medical care. Moreover, the researchers said the abnormal-but-not-TB category also improved the accuracy of their TB-screening algorithm, allowing the model to home in on abnormalities specific to TB.
The “distinction between abnormal but not TB and abnormal and TB was one of the creative solutions that we had” that helped make the model better, said Shruthi Prabhakara, a Google researcher and an author of the study.
To be clear, the authors noted that Google’s system would not be the first AI ever devised to accurately screen for TB. Indeed, the WHO already recommends that such AI systems be used for TB screening. Nevertheless, researchers say adapting systems like this one can help combat that devastating impact of TB all over the world, especially in underserved health-care systems
To test the algorithm, researchers studied some 1,200 patients from four different countries as well as a separate data set of some 1,000 people from a gold-mining community in South Africa. The study was retrospective, meaning that the data in question was collected from medical records, not current patients. Researchers compared the AI’s accuracy with that of nine radiologists from India, where TB is endemic, and five from the United States, where it is not.
In most cases, the AI produced very similar results in terms of both sensitivity and specificity to radiologists. Sensitivity, or true positive rate, is how well a system can correctly identify a person with TB, while specificity, or true negative rate, is how well it can isolate the people who don’t have TB.
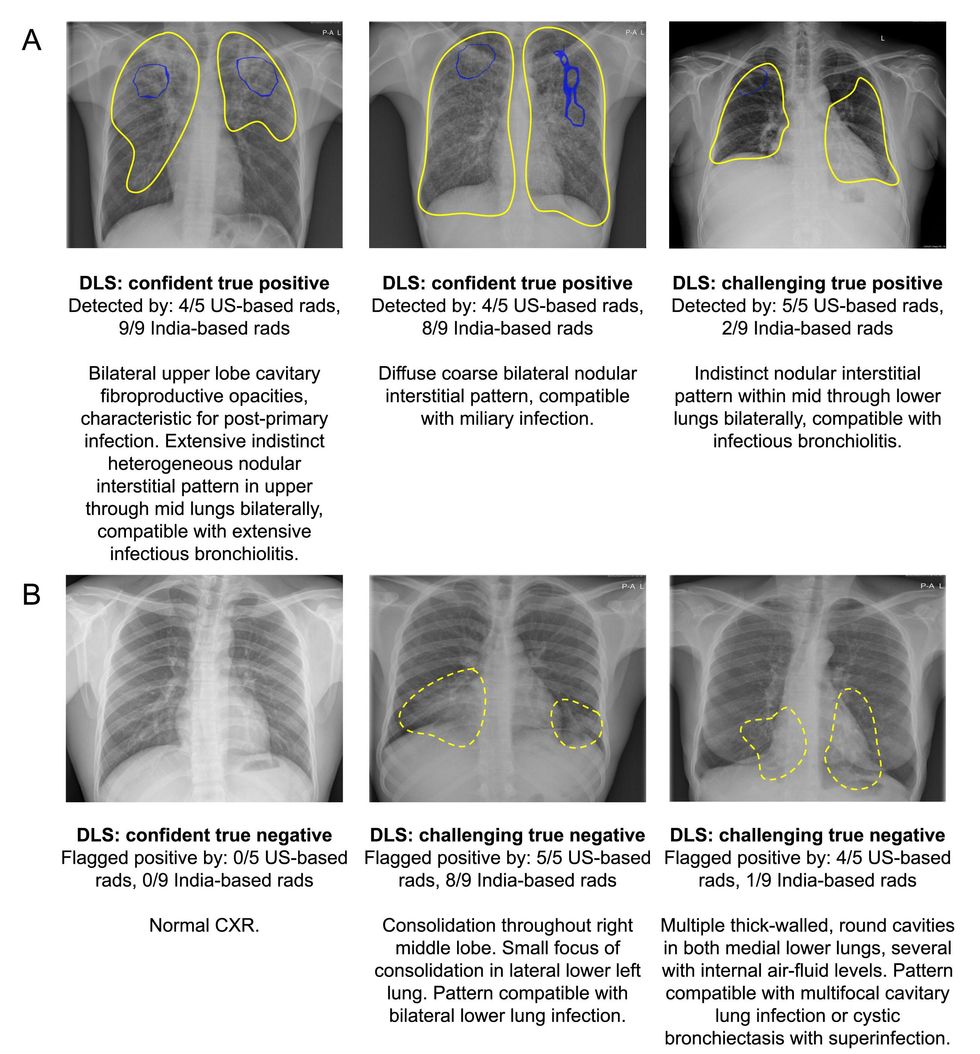 Examples of chest radiographs for which the deep-learning system (DLS) provided the correct interpretation, corresponding to (A) tuberculosis (TB)–positive subjects and (B) TB-negative subjects. Radiological Society of America
Examples of chest radiographs for which the deep-learning system (DLS) provided the correct interpretation, corresponding to (A) tuberculosis (TB)–positive subjects and (B) TB-negative subjects. Radiological Society of America
For most of the data sets, the AI was able to meet WHO requirements for TB screening tests of at least 90 percent sensitivity and 70 percent specificity. Though the AI did not meet these requirements for the South Africa and Zambia data, radiologists also couldn’t meet these standards. An analysis of some of the subgroups involved in the study helps highlight why. For both the AI and radiologists, patients with HIV, who made up most of the patients in the Zambia data set, were more difficult to correctly screen. Many of the false results, the researchers reported, occurred in patients with other lung conditions, which are more prevalent in populations like the South African miners data set.
“There are mimics of TB, which means that there may be things that may look almost like TB on a chest X-ray, which then is not TB,” said Dr. Sanjay K. Jain, a professor at the Johns Hopkins University School of Medicine who studies TB imaging and who was not involved in the study.
Google’s algorithm is not the first AI to use chest X-rays to screen TB patients. As part of a 2021 update to WHO recommendations on screening for TB, the agency looked at three similar technologies—concluding that because the technologies were about as accurate as human radiologists, who are scarce in many areas, health-care systems can use these AIs for TB screening and triage in place of human experts and specialists. Though only a laboratory test can truly diagnose TB, AI systems can screen patients so that only those who are likely to have TB receive lab tests, which are typically more expensive than chest X-rays on their own. However, the researchers also found that while this method can save money, it saves the most when disease prevalence is low, becoming closer to the cost of simply giving everyone a laboratory test as prevalence increases.
The study incorporated diverse data sets but did not incorporate study participants who were current patients.
“I think a study where the system is actually used by the people in the field is a logical next step,” said Dr. Ronald Summers, a radiologist who directs the Imaging Biomarkers and Computer-Aided Diagnosis Laboratory at the National Institutes of Health Clinical Center. In fact, the study’s researchers have already started doing that work, they said.
Although technology similar to the one used in the study already exists, Google researchers said they just want to provide another effective option for this technology. “Our goal is not to go out and try and prove superiority over other products,” said Daniel Tse, a Google researcher and one of the study’s authors.
Jain said that even if the system is not perfect, developing these sort of AI systems is still important.
“This is moving in the right direction,” he said. “I think we should encourage this kind of system.”
Monitoring a Pregnancy at Home with a Smartphone
22 de Setembro de 2022, 18:43 - sem comentários ainda
This article is part of our exclusive IEEE Journal Watch series in partnership with IEEE Xplore.
A pregnancy, while an exciting time for expecting parents, can be riddled with many trips to a doctor’s office in order to monitor the health of the fetus. Currently, the most common method for monitoring the heartbeat of a fetus is through an ultrasound test—which not only requires a visit to the doctor’s office, but the expertise of a trained technician.
In the search for a simpler approach, researchers have developed a novel system that includes a wearable device, smartphone, and algorithm that could offer at-home monitoring of a fetus’s cardiac health. The new algorithm, dubbed Lullaby, is described in a study published on 19 August in IEEE Sensors Letters.
The wearable device involves a patch that’s placed on the abdomen of a pregnant user as well as electrodes that monitor the electrocardiogram (ECG) signals from the fetus. The device also includes a microcontroller which processes the signals and sends them via Bluetooth to a smart phone or watch. Users can then view the data on an app.
However, a major challenge with this type of tech is the fact that continuous ECG monitoring involves a lot of data to process, which has made real-time monitoring with wearable devices challenging. The new Lullaby algorithm addresses this issue.
“Lullaby was made to push the boundaries of the field by creating an algorithm that could process high resolution ECG in real-time and on a wearable device,” explains Daniel Jilani, an undergraduate researcher at University of California Irvine who co-led the development of this technology.
It works by exploiting the fact that a heartbeat has a steady rhythm. It uses this temporal pattern to better distinguish between true and false heartbeats—therefore focusing its computational power more on the heartbeats themselves, rather than the cardiac activity between heartbeats. This reduces the amount of computation required to process the data and extract the fetal heartbeats.
 This fetal cardiac monitoring system uses a patch with electrodes, which record the abdominal ECG signals of a pregnant user. The novel system is currently being developed jointly by Sensoriis inc. and HERO Laboratory.Tai Le
This fetal cardiac monitoring system uses a patch with electrodes, which record the abdominal ECG signals of a pregnant user. The novel system is currently being developed jointly by Sensoriis inc. and HERO Laboratory.Tai Le
In their study, the researchers used a dataset of abdominal ECG recordings to test the Lullaby approach against other existing ECG-processing algorithms, finding it to be nearly seven to 1,000 times faster than these existing options.
“In terms of power, we believe that the algorithm is efficient enough to run continuously [on a smart phone] for days or weeks,” says Jilani. “In terms of RAM memory, the Lullaby algorithm's uses memory on the scale of kilobytes, meaning it can run on memory-limited devices such as microcontrollers and smartwatches.”
The researchers do not yet know how accurate the Lullaby approach is compared to a traditional ultrasound test, but they note that ultrasound devices are less accessible, more expensive, and more difficult to operate than ECG. What’s more, ultrasound tests are done during a visit to the doctor’s office, whereas a wearable ECG device can provide more continuous monitoring as a pregnant user goes about their normal day. Importantly, Jilani notes that this technology could be especially impactful by making fetal heart monitoring more accessible to low-income and disadvantaged communities.
Since this initial study, Jilani says the team has already greatly improved the algorithm to be more accurate and faster than the original version, and they are currently working towards implementing it in a full system. This includes work on a mobile app that can be used on smart phones to support fetal heart monitoring.
They currently have a provisional joint patent on the Lullaby algorithm with the University of California Irvine, and have teamed up with a sponsoring company, Sensoriis Inc., to produce a novel fetal cardiac monitoring system that uses it.
